The typical focused cardiac ultrasound consists of five basic view: parasternal long axis (PLAX), parasternal short axis (PSSAX) mid papillary level, the apical four chamber (A4C), subcostal (SC), and inferior vena cava (IVC). In this section we cover the basic landmarks for probe placement as well as sono-anatomy and aspects of technically adequate image acquisition. For full details of technical adequacy have a look at the American Society of Echocardiography’s guideline.
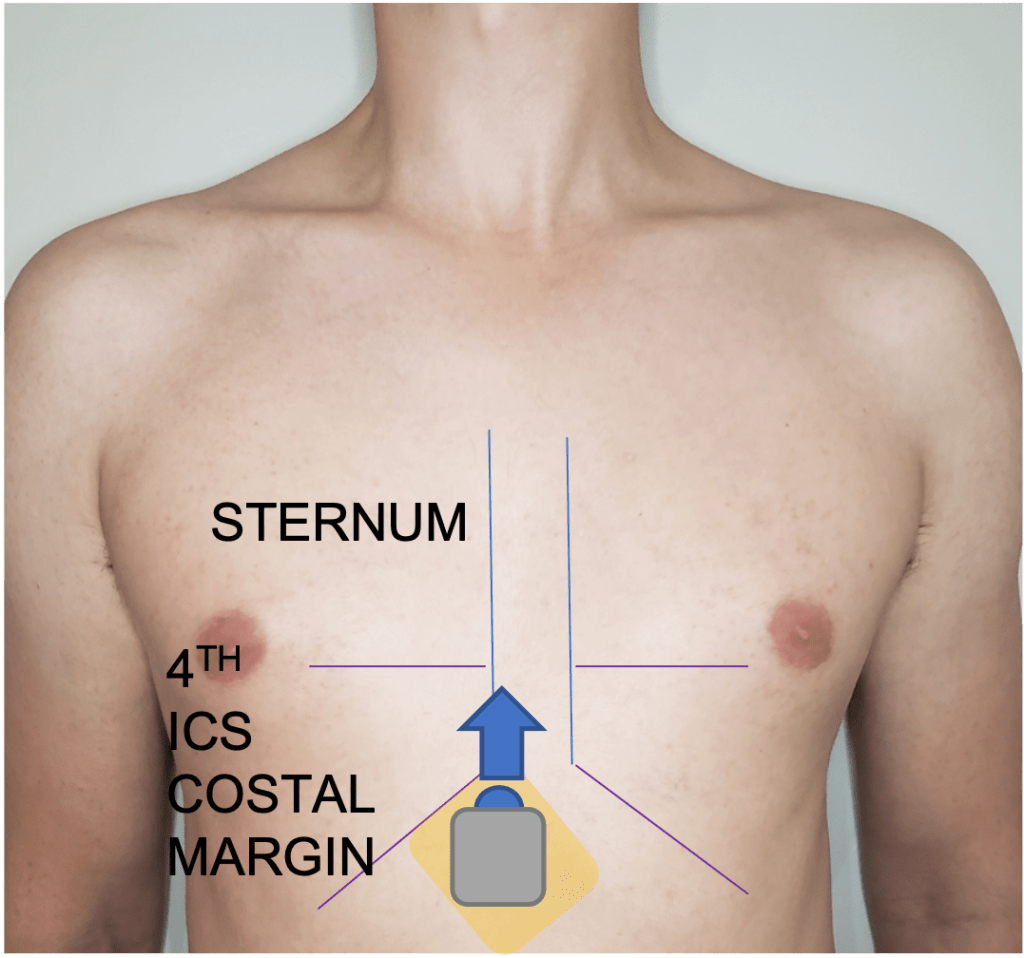
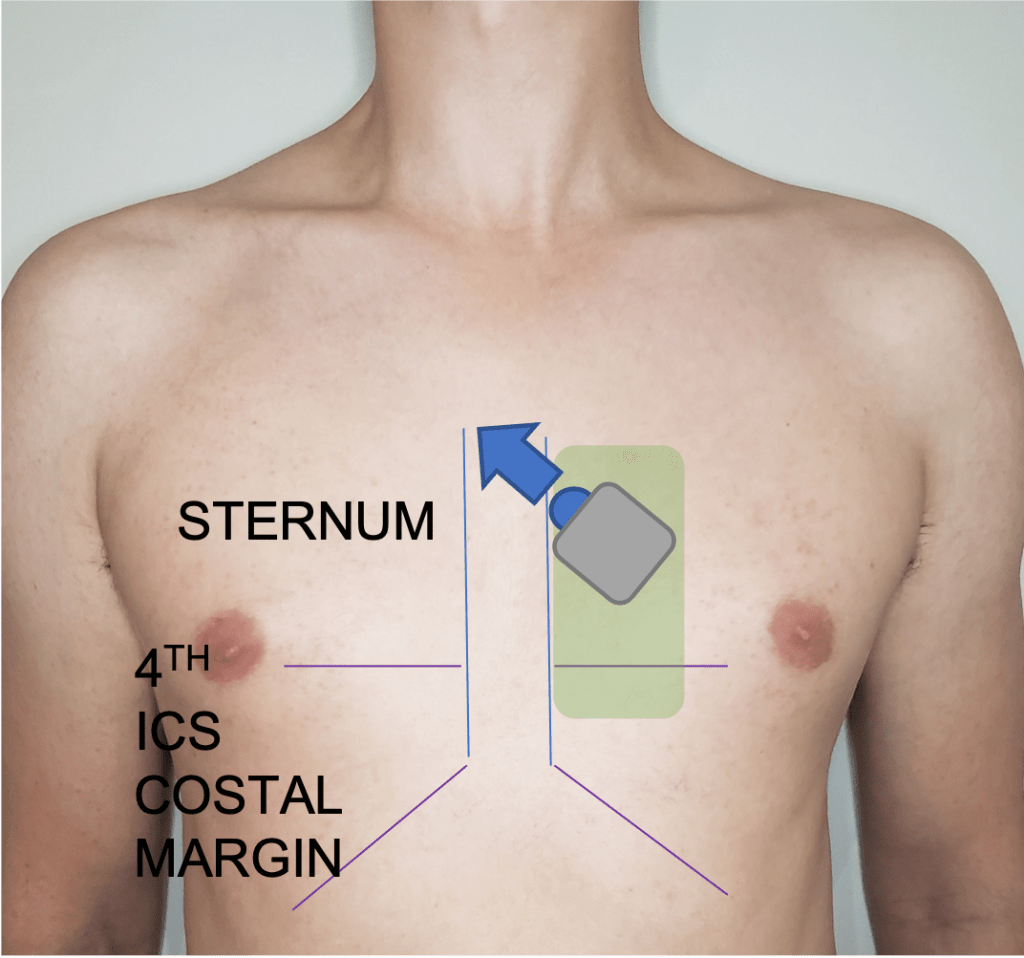
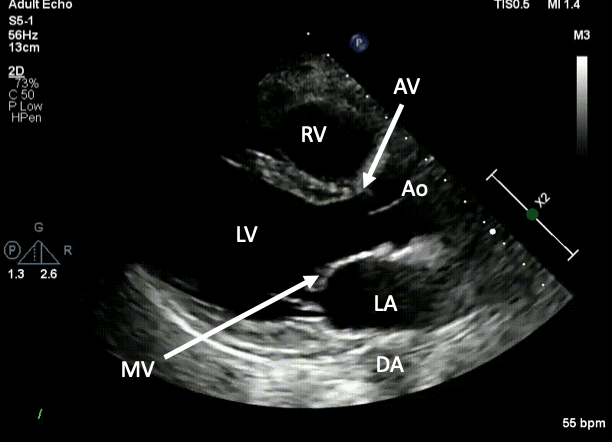
Parasternal Long Axis
Position patient in left lateral decubitus if possible. Typically acquired left parasternal border between the 2-4th interspace with probe marker in the 9-10 o’clock position. Left ventricle should be perpendicular to the transducer. The LV apex should not be visible. MV leaflet tips should be roughly at the center of the image. Ensure sufficient depth to capture the descending aorta. Gross LV function, RV/aortic root/LA dilation, valvular abnormalities, and pericardial effusion are assessable from this view.

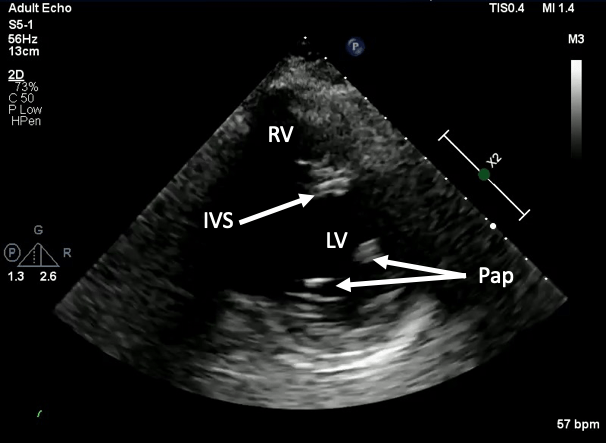
Parasternal Short Axis
Rotate transducer clockwise ~90 degrees from PLAX. For focused assessment we aim to image the LV at the level of the papillary muscle (however the heart can be imaged from apex to the great vessels from this view). The LV should be circular. Aim to capture all LV walls with sufficient depth to visualize the pericardium at the inferior wall. LV function, pericardial effusion, RV hemodynamic effects (e.g. pressure/volume overload), are evaluated from this view.


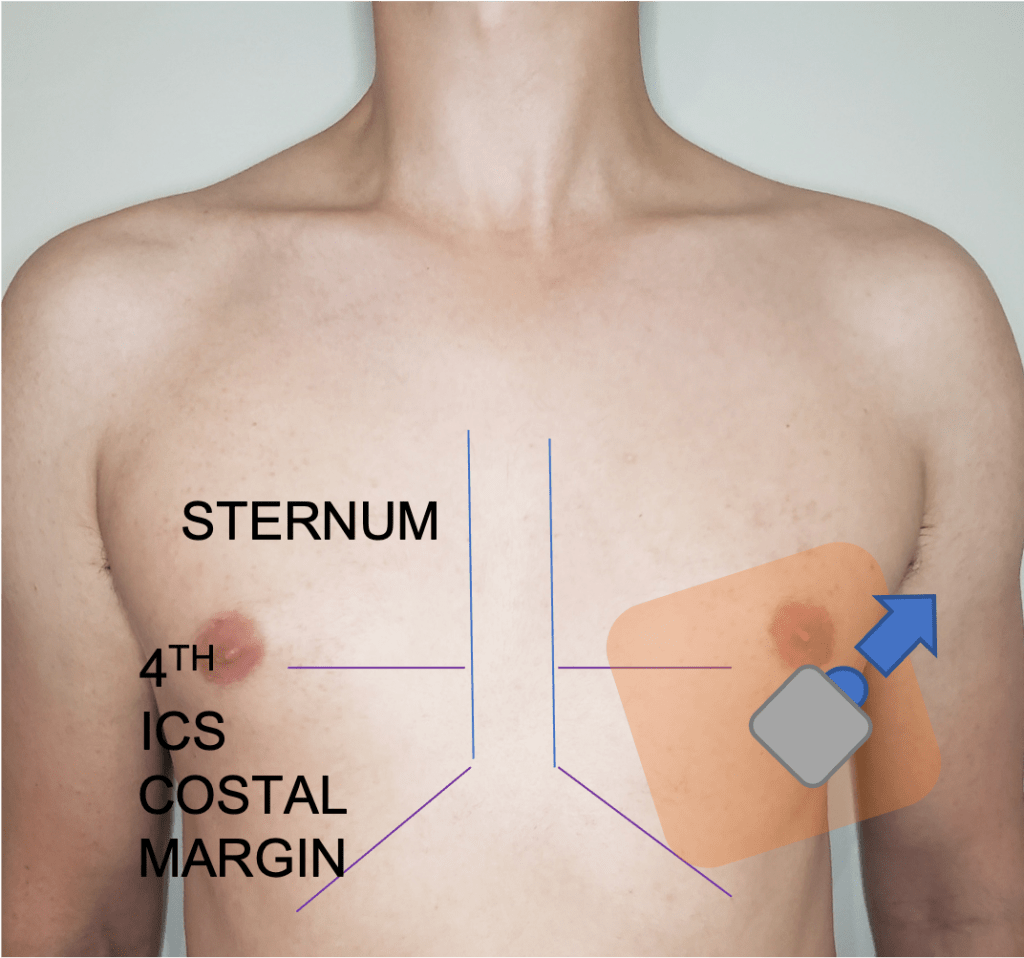
Apical Four Chamber
Place the transducer at the palpated apex, usually 4th-5th interspace midclavicular line, with the probe marker aimed towards the bed; often the final position is between the 2-3 o’clock position. Often you will need the patient in left lateral decubitus and may need to move quite lateral; the midclavicular line is only a starting point. The walls and septa of each chamber should be visualized as well as the tricuspid and mitral valve. LV function is evaluated to a lesser extent, but RV dilation and function are best evaluated here as well as major valvular abnormalities of the MV and TV.


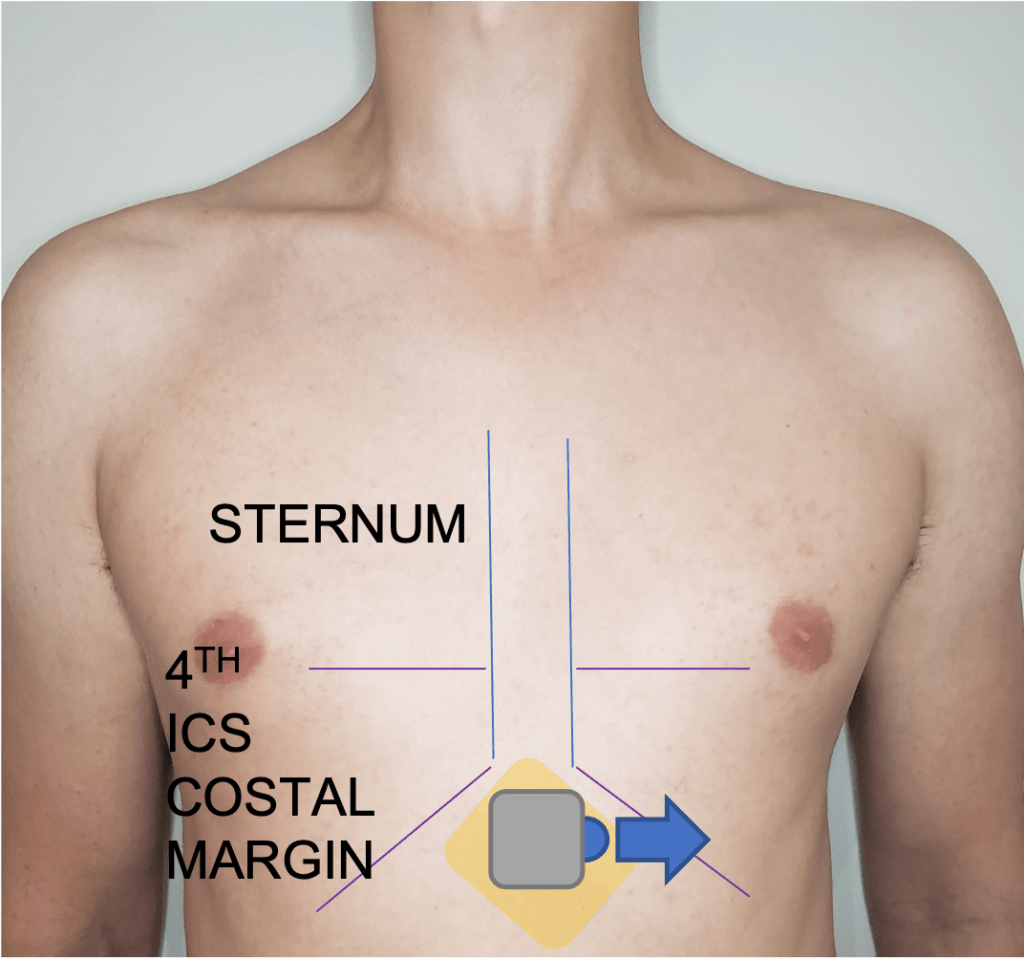
Subcostal
This view is acquired with the patient supine. The probe is placed with the probe marker to the patients left (3 o’clock position) just below the xiphoid process. The four chambers including the TV and MV should be visible. This view is important for assessment of pericardial effusions.

Inferior Vena Cava
This view is acquired with the patient supine. The probe is placed with the probe marker to the patient’s head (12 o’clock position) just below the xiphoid process. In order to be sure the vessel is IVC ensure it is seen draining into the RA with the hepatic vein seen joining just proximal to the atriocaval junction. The IVC is controversial in its clinical application for management decisions but is generally an accurate estimation of right atrial pressure.