Indications
Inferior vena cava (IVC) ultrasound consists of measurement of diameter of the IVC during different phases of the respiratory cycle and the degree of collapsibility/distensibility used as a surrogate measure of right atrial pressure. Think of it as a more objective version of the JVP
Handle with caution: The IVC scan is one of the more diagnostically controversial scans. In the early days of POCUS the IVC rose to prominence as a straightforward scan that would deliver us the answer to the age old question of what a patient’s “volume status” was and if they were “volume responsive”. This promise has not born out in reality and when rigoursly studied it is not a reliable marker of volume responsiveness and it has an abundance of caveats even when used as a indirect measure of right atrial pressure.
The bottom line: As with any POCUS the scan the IVC should never be used in isolation and should be incorporated along side the history, physical, and other POCUS scans to assist with diagnosis.
As for our two cents, we suggest that IVC be used for the same indications as one would assess the JVP but with a firm appreciation of the significant limitations of the scan.
Acquisition
Begin by using either the curvilinear or phased area probe; the IVC is a deep structure and therefore is best visualized with a low frequency transducer.
The IVC can be imaged from 2 places: the epigastrium (left) or R4 zone (right). We consider R4 a “rescue view” to be used when the epigastric is not accessible and to be used with caution as it is a non-standard view.

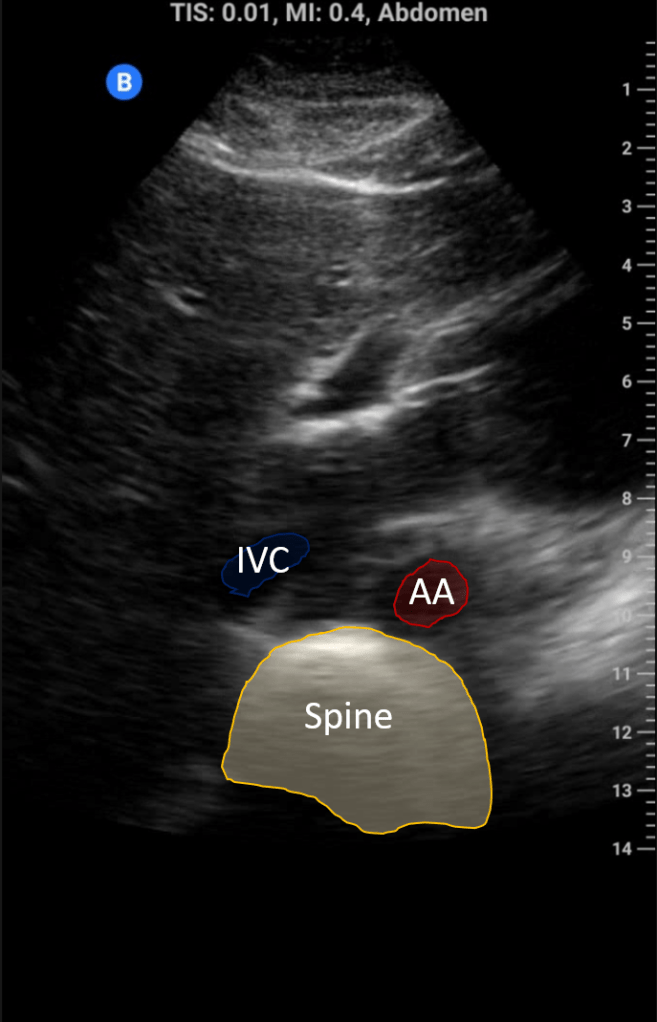
Begin in transverse; you should see the left lobe of the liver below this 2 tubular structures (IVC and aorta) and the spine below. Center the IVC and then rotate to the longitudinal view.
In the spontaneously breathing patient measure IVC maximal IVC diameter 2 cm distal to the right atrial junction at end expiration; in intubated patients measure at maximal inspiration. Repeat the measurement at end inspiration (or expiration in intubated patients) and calculated the collapsibility using the formula below:


This is a precise way do to this but cumbersome; it is acceptable to “eyeball” the collapsibility after measuring the maximal diameter and stratify to collapsing > or < 50%.
Interpretation
The below table provides a rough guide on estimating right atrial pressure based on IVC diameter and collapsibility:

The IVC is diameter is dependent on intra-abdominal pressure, changes in intrathoracic pressure and the complex relationship to right heart filling, right ventricular systolic function, vessel compliance of the IVC itself. All these factors can influence IVC size and distensibility and must be considered in its interpretation.
Pearls
A common challenge in imaging the IVC is confusion with the aorta. Here are some helpful distinguishing features to avoid such an error:
IVC
- Right side
- Thin walled
- Diameter changes with respiration
- Hepatic vein drains into it
- Connects to the right atria
- Surrounded by liver
Aorta
- Left side
- Thick walled
- No change in diameter with respiration
- No hepatic vein present
- Passes “under” the heart
- No liver parenchyma below
Pitfalls
Imaging off-axis: One of the factors that makes IVC measurement so fraught is the challenge of trying to measure the diameter of a tubular structure. If you do not measure the IVC through the middle you “side-wall” the vessel leading to an underestimation. It is therefore important to make sure you are parallel to the course of the vessel and measuring at its true maximum diameter.