Indications
In this tutorial we focus on lower extremity ‘2 point’ compression ultrasound. This is used for the detection of deep vein thrombosis (DVT) and can either employed in a patient with typical symptoms of lower extremity pain/edema or as part of a larger protocol in the setting of respiratory failure or shock where pulmonary embolism is suspected (e.g. RUSH/BLUE protocol) in combination with thoracic/cardiac imaging. Performance of vascular ultrasound of any kind requires solid knowledge of underlying anatomy and in all but the most experienced of practitioners when it comes to the detection of thrombosis should be used as a ‘rule-in’ tool only.
Acquisition
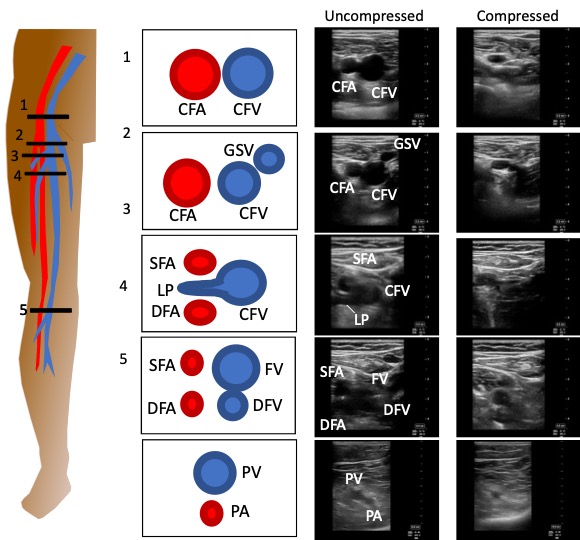
The 2 point compression protocol refers to two areas of focus; the inguinal region and popliteal fossa. The protocol itself includes 5 anatomic locations between these areas and has between 86-100% sensitivity and 96-99% specificity for the detection of clots in acute care patients.(1,2)
A linear probe is utilized and is in transverse orientation throughout the protocol with the probe marker to the patient’s right. The patient should be supine with their hip externally rotated (in a ‘frog-leg position) and the knee partially flexed.
The figure below shows the approximate anatomic location of probe placement. Images in the inguinal region aim to survey the common femoral vein and its major branch points which are at higher risk to develop thrombosis: common femoral vein (CFV), branch point of the greater saphenous vein (GSV), lateral perforator (LP), and deep femoral (DFV)/femoral vein (FV). Scanning the popliteal fossa aims to only interrogate the popliteal vein but it should be traced several centimetres above the popliteal fossa and down to the level of the trifurcation to exclude above knee clot.
We do recommend as well scanning down about 5 cm from the branch point of the GSV and the DF/FV compressing at multiple points along their course.
The compression maneuver is the method for detecting clot if it is not immediately visible OR if it is very acute and may be almost completely anechoic. Firm perpendicular pressure is applied until the lumen of the vein is completely obliterated. Maintaining the vein on screen and at the target location can be quite difficult and requires solid hand anchoring and hand-eye coordination.
In comprehensive departmental scans of the lower limb the whole leg is scanned from common femoral to below the trifurcation including Doppler and augmentation maneuvers (i.e. Doppler assessment with calf squeeze); we forgo these in POCUS.
Interpretation
The outcomes of a DVT scan can be positive, negative, or indeterminate. Below are examples of each.

Negative: In this clip thrombus is definitively excluded as there is complete collapse of the lumen of the common femoral vein (vessel on the left). The common femoral artery can be seen remaining partially patent ad pulsating on the right. There is no need to collapse the artery.

Positive: In this clip even before compression a hypoechoic structure within the lumen of the common femoral vein at the level of the lateral perforator can be seen but is PROVEN with in ability to compress. This is diagnostic for thrombus.
Positive: In this case we are looking at a completely occluded popliteal vein (with no compression applied) and on the immediate right a branch vessel as well. In complete occlusions it might be difficult to discern the vein especially if it is more chronic and more isoechoic with the surrounding tissue. This highlights why it is so important to visualize the artery as it assists with localization.
Indeterminate: In this clip we do not see compression of the femoral vein or deep femoral vein but we cannot easily visualize a clot either. There is significant longitudinal shifting caudally of the probe evidenced by the branch point to the deep femoral vein coming into view midway through the clip. Lack of compressibility is most often due to inadequate compression BUT a very acute clot (which can be completely anechoic) cannot be excluded. In this scenario a comprehensive radiology exam is mandated as a next step to resolve this if optimization of positioning and compression maneuver does not help.
Pearls/Pitfalls
In this section we review some of the additional maneuvers and false positives for clots in the deep vein system of the lower extremity.
The primary pitfall of the 2 point approach is just that; it is 2 points and though its sensitivity is generally quite good you will invariably miss some DVTs inparticular it does not interrogate the iliac region at all and there is the possibility to miss clots between the popliteal fossa and the bifurcation of the femoral and deep femoral vein. Additionally there is the technical challenge in the popliteal fossa whether the hamstring tendons can impair contact with the fossa especially in smaller individuals.
Below we will highlight some other technical challenges and rescue maneuvers as well as potential false positives.
Transducer movement: By far the greatest challenge of performing compression ultrasonography is maintaining a consistent anatomic position and screen view. In this clip we are the level of the bifurcation of the femoral and deep femoral vein with the superficial femoral artery seen in the near field and deep femoral artery below. The clip appears negative but its hard to know as the femoral vein slides entirely off the screen. The key is to anchor your transducer hand to the patient and use slow compression keeping the vessel of interest centered on the screen; this is a tough skill to master.
Colour Doppler: The use of colour Doppler can be a helpful adjunctive maneuver for a challenging scan. If there is slow continuous colour signal within the lumen of the vein a clot is less likley, in plane example of the this is shown in the image on the left where low velocity colour is seen occupying the lumen of the common femoral vein (vessel on the right). In the image below a side by side comparison of B-mode and colour doppler of a clot at the branch point of the femoral and deep femoral vein. In this case of clot there is absent signal within the clot and swirling turbulent flow around the edges of the clot due to the intermittent occlusion of part of the vessel wall as the clot floats back and forth in the lumen. But beware, Doppler signal is extremely dependent on being sufficiently parallel to flow, having the Nyquist limit (max/min velocities of the color scale), and gain all set appropriately so proceed with caution when using this as a rule in tool.
Spontaneous echo contrast: In this clip you might notice the femoral vein (screen left) has echogenic material in the lumen of the vein BUT it fully compresses. This is a false positive for clot and is seen most often in low flow states and is a reasonably specific sign for right heart failure . The mechanism is as blood flow slows and RBCs are more concentrated in place they become more echogenic and act like a contrast agent (hence the name).
Valves: A common false positive for clot is the presence of a valve. This is a normal vein structure to prevent blood from refluxing backward. The green arrows show the attachment points of the valve between the greater saphenous vein and common femoral vein which appears a lacey hyper-echoic structure within the vessel lumen.
Lymph Nodes: In the inguinal region is frequent location for findings lymph nodes; an example is shown with the green arrow in the image on the left. They will appear similar in echogenicity to thrombi and will non-compressible and can be a false positive. They can be easily excluded as they will have rounded borders with a hyperechoic central hilum without connection to the vasculature of the region.
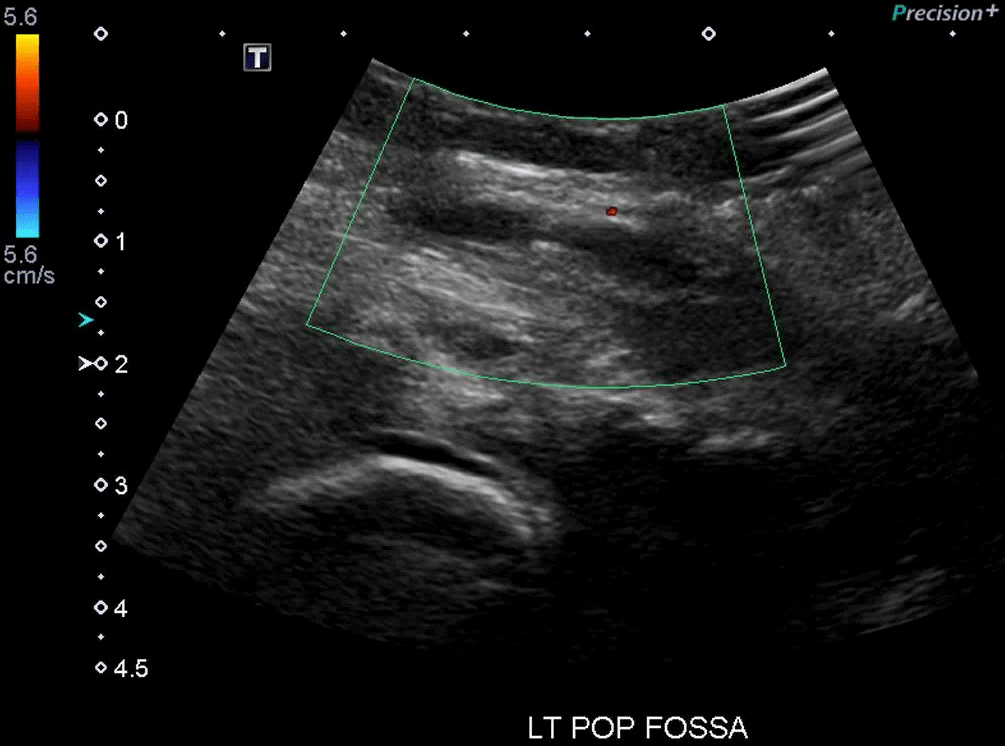
Baker’s Cysts: A Baker’s cyst forms in the popliteal fossa from an accumulation/extrusion from the synovial capsule of the knee and can be a false positive for DVT as they are anechoic and non-compressible. In the image on the left the anechoic structure within the Doppler box is a Baker’s cyst. Similar to lymph nodes they are not continuous with surrounding vasculature and have discrete rounded edges.
References
- Crisp JG, Lovato LM, Jang TB. Compression ultrasonography of the lower extremity with portable vascular ultrasonography can accurately detect deep venous thrombosis in the emergency department. Annals of emergency medicine. 2010 Dec 1;56(6):601-10.
- Kory PD, Pellecchia CM, Shiloh AL, Mayo PH, DiBello C, Koenig S. Accuracy of ultrasonography performed by critical care physicians for the diagnosis of DVT. Chest. 2011 Mar 1;139(3):538-42.