Indications
One of the more straightforward cardiac assessments is evaluation for pericardial effusion owing to the lower learning curve of subcostal view acquisition where effusions are most often best visualized. The general indications are undifferentiated dyspnea, hypotension, and/or chest pain.
Acquisition
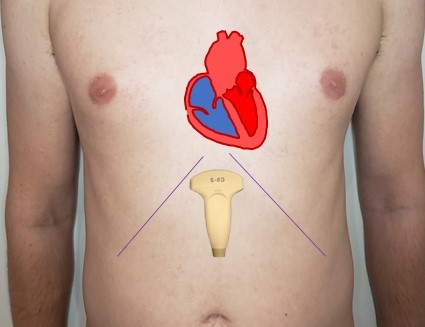
Use the phased array or curvilinear probe (though due to its smaller footprint and superior motion capture phased array is always preferred). If using the phased array with a cardiac exam preset, the screen marker will be on the RIGHT. Therefore, make sure the probe marker is to the patient’s LEFT. If using the curvilinear probe have the probe marker to the patient’s right. Identify the xiphoid process and move 2 cm down, then holding the probe at a 45 degree angle apply firm pressure and aim the beam towards the left shoulder. Once you have identified the heart fan (tilt) up and down scanning fully from anterior to posterior ensuring you are able to see the whole free wall of the RV to the apex.


Interpretation

If you see anechoic space “above” the RV free wall (i.e in the near field) and right atria that becomes larger as you scan posteriorly this is a positive scan for effusion. Ideally you would confirm with a second cardiac view but with moderate (1-2 cm) or large (>2 cm) this is not always necessary. This image shows a moderate pericardial effusion.
Pearls
Attempting to image the heart from directly below the xiphoid process is frequently limited by gas within the stomach. In this case move to the right and down and use the left lobe of the liver as an “acoustic window”. The liver does not scatter the ultrasound beam and therefore provides a clear path to the heart.

You can use the subcostal view to quickly transition to the IVC. Simply centre the right atrium in the screen and then rotate the probe 90 degrees clockwise to move into the longitudinal axis of the IVC.
Pitfalls
Effusion or epicardial fat: A common false positive for effusion is the epicardial fat pad which can appear quite hypoechoic and can sometimes be quite large. Features to help distinguish epicardial fat pad versus effusion are 1) epicardial fat moves with the heart and 2) becomes smaller as you scan posteriorly; an effusion, unless loculated, will generally enlarge as you move posteriorly.

Effusion size: A small effusion can cause tamponade and a large effusion may not. More important than the size is the rate of accumulation. The pericardial sac has the ability to accommodate several litres of fluid, which if built up slowly even VERY large effusions will not cause tamponade. Therefore if you are concerned about tamponade and there is an effusion on ultrasound, your next move needs to be calling for help; using traditional physical examination assessing for significant pulsus paradoxus with a manual BP cuff is helpful to communicate urgency. There are many echocardiographic signs that can also suggest tamponade but outside of highly advanced users these are usually in the realm of cardiology as opposed to POCUS and remember tamponade is CLINICAL DIAGNOSIS. For example, the image on the right shows a moderate effusion but this patient had a pulsus of 18 with a resp rate of 40. They underwent pericardiocentesis and improved with drainage of just 20 ccs!